|
PARTNERSHIPS FOR ENHANCED ENGAGEMENT IN RESEARCH (PEER) HEALTH
Cycle 1
Reducing Loss-to-Follow-Up Among HIV-exposed Infants in Central Mozambique Principal Investigator: Lucia da Costa Vieira, Beira Operations Research Center (CIOB) NIH-Supported Collaborator: James Pfeiffer, University of Washington Title of NIH Award: Early ART Initiation Among HIV-positive Pregnant Women in Central Mozambique
Project Dates: October 2013 - September 2020
Project Overview
Diagnosis and care for children exposed to HIV remains a major challenge throughout the developing world. Identifying HIV-exposed infants, diagnosing HIV infection and starting HIV-positive infants on treatment requires a well-coordinated care cascade. This care cascade has proven challenging in many developing countries, including Mozambique. Preliminary research suggests that the current system in Manica and Sofala Provinces in Mozambique retain less than 50% of HIV-exposed infants in appropriate care. Failure to properly identify and treat HIV-positive infants contributes to childhood morbidity and mortality. In addition, the problem of vertical HIV transmission is compounded by limited access to family planning services for HIV-positive women. In Manica and Sofala Province, only 13% of women use family planning methods. In 2012, the WHO adopted a “test-and-treat” approach, referred to as “Option B+”, that seeks to streamline the treatment cascade by starting ART in all HIV-positive women at the time of diagnosis in antenatal care services (ANC) regardless of CD4 count to avoid delays and multiple visits that contribute to LTFU. The new Option B+ approach has been adopted by the Ministry of Health (MoH) in Mozambique and is in the early phases of implementation. In Mozambique, antenatal care (ANC) and HIV testing coverage is high but there is substantial loss-to-follow-up (LTFU) at successive stages in the treatment cascade, limited counseling for women and many barriers to actively tracking those women lost to follow-up. Early Ministry of Health data suggests significant challenges remain for long-term adherence for women started on ART via the new Option B+ framework in Manica and Sofala provinces and throughout Mozambique. This project will build off an existing NIH grant– a clustered (facility) randomized controlled implementation science trial to improve the rollout of “Option B+”, in which HIV positive pregnant women initiate ART during pregnancy regardless of CD4 count and continue treatment for life. The objectives of this study are to identify causes of loss-to-follow-up of HIV-exposed infants in care cascade and barriers to family planning access and then design and implement an intervention that will increase the proportion of infants tested for HIV and enrolled in pediatric HIV care as well as increase the proportion of HIV-positive women receiving family planning services. This study will identify causes of loss-to-follow-up of HIV-exposed infants in the care cascade and barriers to family planning access through qualitative and quantitative formative research. In close collaboration with the Ministry of Health, the investigators will then design an intervention based on formative research findings which utilizes three core components: enhanced system tracking and linkages for HIV-exposed infants, improved counseling for infant caregivers regarding appropriate care for HIV-exposed and HIV-positive infants, and integration of family planning counseling in well child, postpartum and child at risk clinic visits. Once this intervention is developed, the study team will implement the intervention through a clustered (facility-level) randomized controlled trial using a stepped-wedge design to test the effectiveness of the intervention. This project has the potential to influence current USAID and Ministry of Health practices by testing an approach that could be scaled up at similar facilities throughout Mozambique that suffer similar challenges with loss-to-follow-up of HIV-exposed infants and poor contraception access.
 | 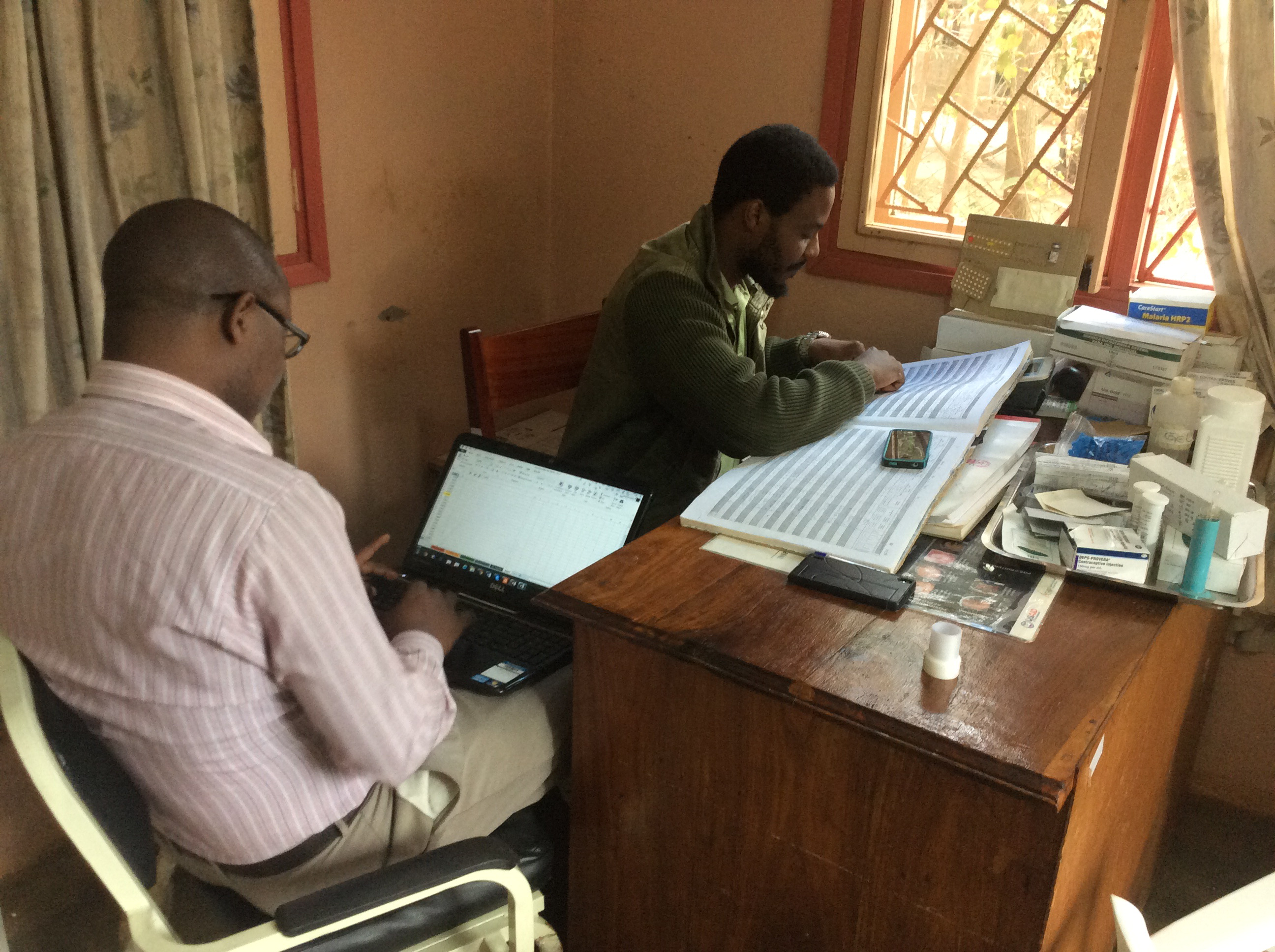 | | | |
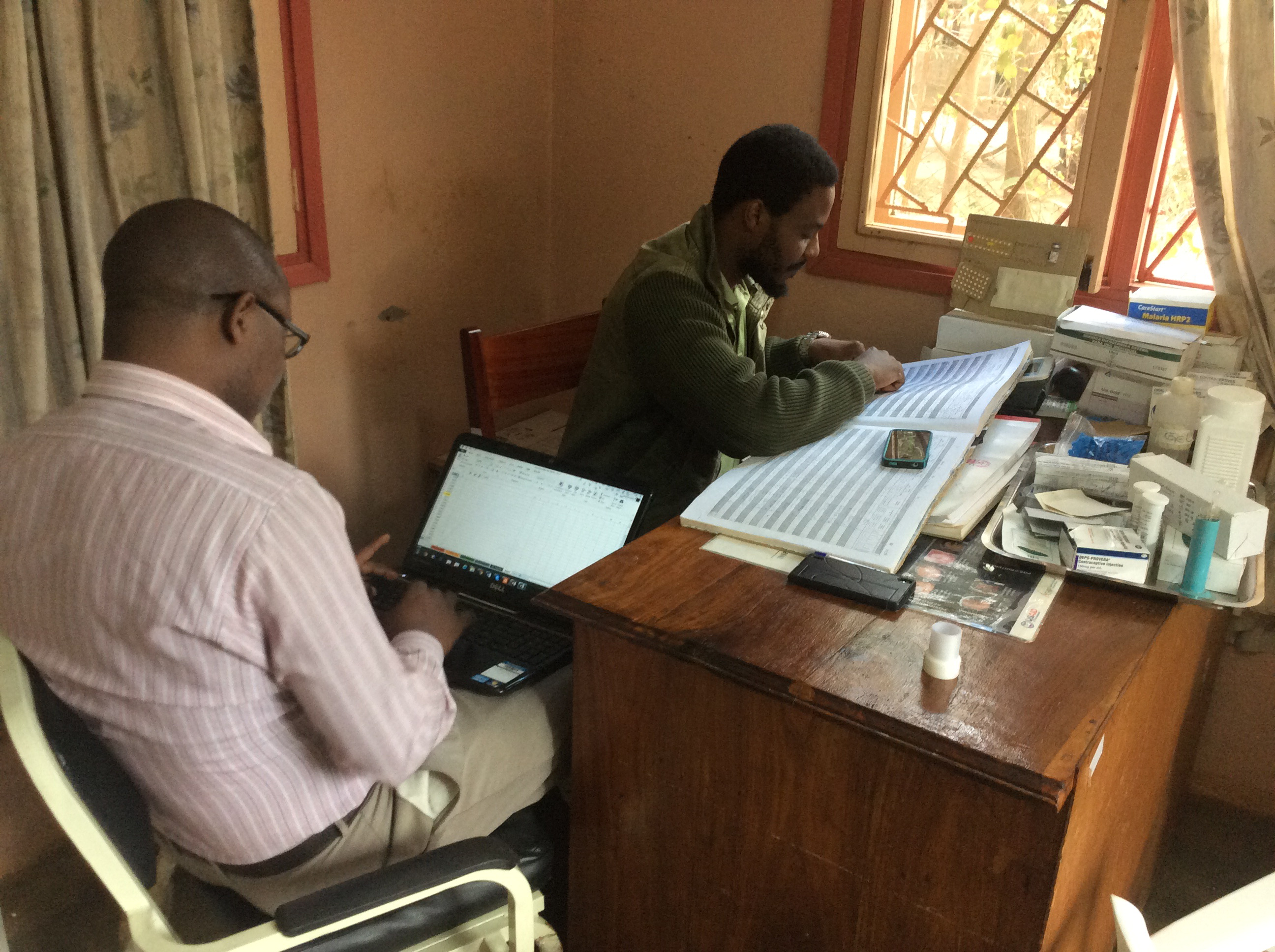
Final Summary of Project Activities
This project has come to a close and proved to be a success in a informing government policy makers on methods to reduce follow-up loss of HIV exposed infants in the country. The intervention sought to improve the retention of the exposed children who have initiated Highly active antiretroviral therapy (HAART) at healthcare facilities and strengthen the link between CPP (post-partum clinic) visits and CCR (children at risk care). The study used community health workers to help the health centers track exposed children and their mothers, as well as cell phones to remind them to return to the health center and to find them if they do not return. The team conducted interventions in six healthcare facilities, arranging numerous Mother-to-Mother group meetings total, working out of each health unit. These aim to share information, challenges, and provide peer-to-peer mentoring, as well as knowledge transfer from health facility staff to mothers at risk. The team also met with study staff at each facility, as well as provided trainings to health professionals on how to follow-up children who were exposed to HIV.
To strengthen the quality of ARV programs in Manica and Sofala provinces, the study team conducted several meeting with the key DPS (Health Provincial Directorate) and other leaders of mother and child and HIV programs about the intervention and the lessons learned throughout the implementation of the research. The health centers in these provinces were receptive to the project results and have implemented the intervention for reducing loss-to follow-up among HIV exposed infants as standard practice. In Maputo dissemination was conducted at the MoH National Directorate of Public Health board meeting. By meeting with all heads of the public health departments, the team was able to transmit the results of the outcome to those who are the key policy makers and have the power to change health policy. The team was pleased to receive the news that the Health Ministry is starting HAART in CCR, which was one of the main recommendations to the Ministry of Health. The team also organized the first CIOB Conference on maternal and child health. The conference was held in the Manica province and all institutions and NGOs operating in the area of maternal and child health were invited to submit their work. Additionally, every three years the Mozambique MoH (Ministry of Health) organizes a national health conference. The team presented the formative results in 2015 and intervention results in 2018. PublicationsVieira, Lúcia et al. “HIV-exposed infant follow-up in Mozambique: formative research findings for the design of a cluster randomized controlled trial to improve testing and ART initiation.” BMC health services research vol. 20,1 226. 18 Mar. 2020, doi:10.1186/s12913-020-5051-8 |